Understanding when to avoid using a cold compress is crucial for effective injury management and therapeutic care. While cold therapy remains a cornerstone of acute injury treatment, certain medical conditions and circumstances make cold compress application potentially harmful or counterproductive. Healthcare professionals and individuals alike must recognize these contraindications to prevent complications and ensure optimal healing outcomes. This comprehensive guide explores the specific scenarios where cold compress therapy should be avoided, alternative treatment approaches, and best practices for safe therapeutic cooling applications.

Medical Conditions That Contraindicate Cold Compress Use
Circulatory System Disorders
Individuals with compromised circulation should exercise extreme caution when considering cold compress therapy. Peripheral vascular disease significantly impairs blood flow to extremities, making patients particularly vulnerable to cold-related tissue damage. The application of cold temperatures can further constrict already narrowed blood vessels, potentially leading to tissue necrosis or prolonged healing times. Raynaud's phenomenon presents another significant contraindication, as cold exposure triggers severe vasoconstriction that can cause painful episodes and tissue damage.
Diabetes mellitus often involves peripheral neuropathy and compromised circulation, creating a dangerous combination when cold compress therapy is considered. Diabetic patients frequently experience reduced sensation in affected areas, preventing them from detecting excessive cold exposure that could cause tissue damage. Additionally, their compromised healing capacity means that any cold-related injury may progress more severely and heal more slowly than in healthy individuals.
Neurological Conditions Affecting Sensation
Patients with sensory neuropathy face significant risks when using cold compress applications without proper supervision. The inability to accurately perceive temperature changes eliminates the body's natural protective mechanism against excessive cold exposure. Spinal cord injuries that affect sensory pathways create similar risks, as patients may not feel the intensity of cold applications that could cause tissue damage.
Multiple sclerosis and other demyelinating diseases can impair temperature sensation and thermoregulation, making cold compress use potentially dangerous. These conditions often involve unpredictable symptom patterns, and cold exposure might exacerbate certain neurological symptoms or trigger symptom relapses in susceptible individuals.
Age-Related Considerations for Cold Compress Avoidance
Pediatric Population Vulnerabilities
Very young children, particularly infants and toddlers, require special consideration regarding cold compress applications. Their developing thermoregulatory systems cannot adequately respond to cold stress, making them vulnerable to hypothermia even from localized cold applications. Additionally, young children cannot effectively communicate discomfort or pain associated with excessive cold exposure, increasing the risk of tissue damage.
The thinner skin and higher surface area to body mass ratio in pediatric patients increases heat loss rates during cold compress therapy. This physiological characteristic means that what might be a safe cold compress duration for adults could pose significant risks for children. Healthcare providers must carefully consider these factors and often recommend alternative treatment approaches for young patients.
Geriatric Considerations
Elderly patients present unique challenges for cold compress therapy due to age-related physiological changes. Decreased skin thickness, reduced subcutaneous fat, and compromised circulation make older adults more susceptible to cold-related injuries. Additionally, many elderly patients take medications that affect circulation or temperature regulation, further increasing their vulnerability to adverse effects from cold compress applications.
Cognitive impairment in elderly patients can prevent proper communication about discomfort levels during cold compress treatment. Dementia and other cognitive disorders may impair the patient's ability to recognize or report excessive cold exposure, necessitating careful supervision or avoidance of cold therapy altogether.
Specific Injury Types Requiring Alternative Treatment
Open Wounds and Surgical Sites
Fresh surgical incisions and open wounds represent absolute contraindications for direct cold compress application. Cold temperatures can significantly impair the wound healing process by reducing cellular metabolic activity and limiting blood flow to the affected area. The compromised circulation associated with cold exposure delays the delivery of nutrients and immune cells essential for tissue repair and infection prevention.
Infected wounds require particular caution, as cold compress applications can mask important clinical signs of infection progression. The vasoconstriction induced by cold therapy may temporarily reduce visible signs of inflammation, potentially delaying necessary medical intervention and allowing infections to progress unchecked.
Chronic Pain Conditions
Certain chronic pain conditions may be exacerbated by cold compress therapy rather than relieved. Fibromyalgia patients often experience increased pain and stiffness when exposed to cold temperatures, making cold compress applications counterproductive. Arthritis sufferers may find that cold therapy increases joint stiffness and reduces mobility, particularly during flare-ups or in cold weather conditions.
Complex regional pain syndrome represents another condition where cold compress therapy should be avoided. The hypersensitivity characteristic of this condition means that cold applications can trigger severe pain responses and potentially worsen the underlying pathophysiology. Alternative warm therapy or other non-thermal interventions often prove more beneficial for these patients.
Medication Interactions and Contraindications
Blood Thinning Medications
Patients taking anticoagulant medications face increased bleeding risks that can be exacerbated by improper cold compress applications. While cold therapy typically helps control bleeding through vasoconstriction, the combination of blood thinners and cold applications requires careful monitoring to prevent complications. Extended cold compress use in anticoagulated patients may mask ongoing bleeding or create conditions that lead to tissue damage.
Antiplatelet medications similarly affect the body's hemostatic mechanisms, potentially complicating cold compress therapy. Healthcare providers must consider these medication interactions when recommending cold therapy and may need to modify treatment protocols or suggest alternative approaches for patients on these medications.
Vasodilating and Vasoconstricting Medications
Medications that affect vascular tone can significantly alter the body's response to cold compress applications. Beta-blockers may impair the normal vasoconstrictive response to cold, potentially reducing the therapeutic effectiveness of cold therapy while maintaining the risk of tissue damage. Calcium channel blockers and other vasodilating medications can create similar complications.
Conversely, medications that cause vasoconstriction may amplify the circulatory effects of cold compress therapy beyond safe limits. The combination of pharmaceutical vasoconstriction and cold-induced vessel narrowing can create dangerous reductions in tissue perfusion, particularly in patients with existing circulatory compromises.
Environmental and Situational Contraindications
Extreme Temperature Environments
Cold compress applications become particularly risky in extremely cold environmental conditions. When ambient temperatures are already low, additional cold therapy can overwhelm the body's thermoregulatory mechanisms and lead to systemic cooling or localized tissue damage. Outdoor workers or individuals in cold climates may need to avoid cold compress therapy during certain weather conditions.
High-altitude environments present unique challenges for cold compress use due to reduced atmospheric pressure and altered circulatory responses. The combination of altitude-related physiological changes and cold therapy may create unexpected complications or reduce treatment effectiveness.
Activity-Specific Considerations
Athletes participating in cold-weather sports face particular risks when using cold compress therapy immediately before competition. The combination of environmental cold exposure and therapeutic cooling can impair muscle function, reduce reaction times, and increase injury risk. Pre-competition cold compress applications should be carefully timed and monitored to avoid performance decrements.
Occupational settings involving cold environments or repetitive cold exposure may contraindicate additional cold compress therapy. Workers in refrigerated environments, for example, may already experience significant cold stress that would be dangerously compounded by therapeutic cold applications.
Alternative Treatment Approaches
Heat Therapy Applications
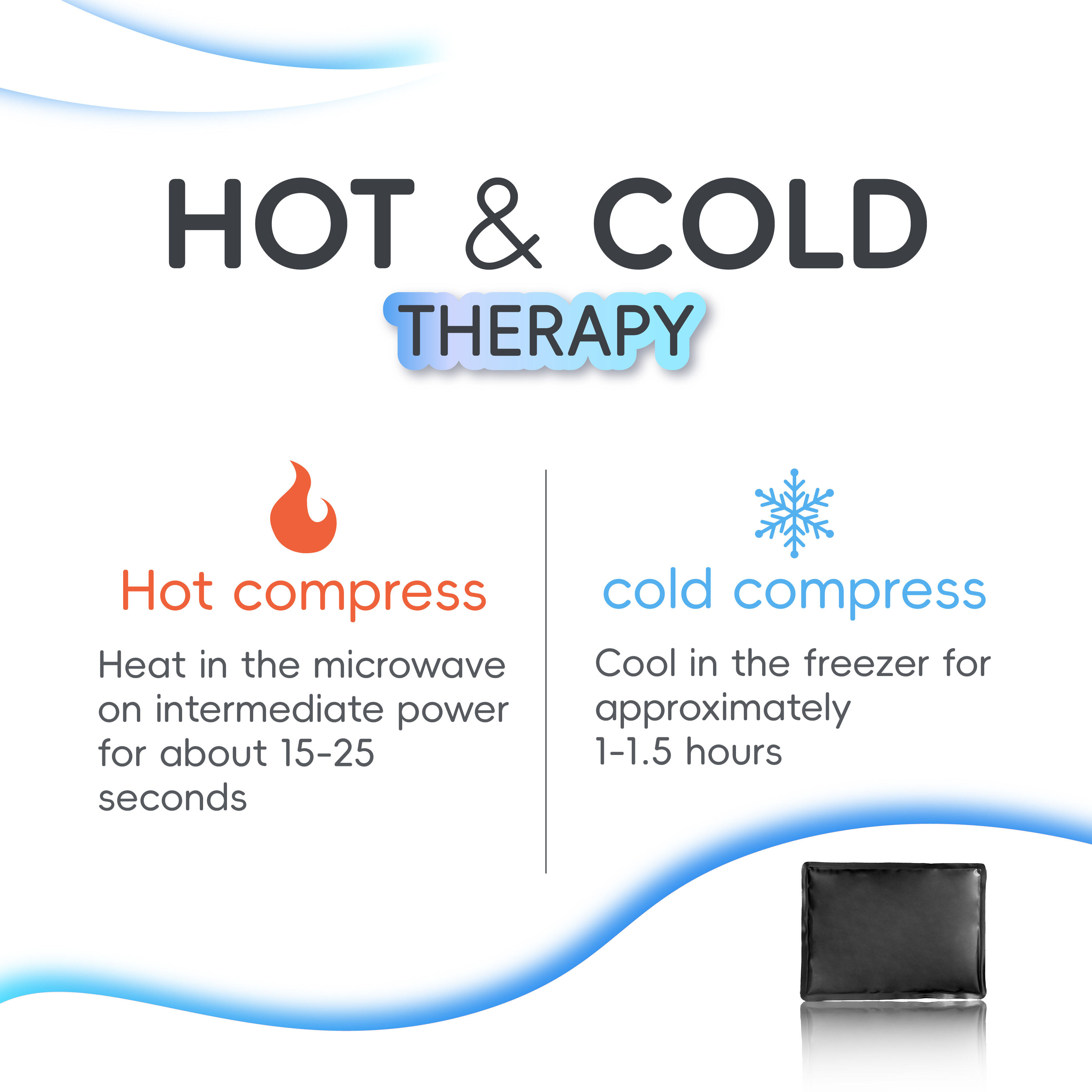
When cold compress therapy is contraindicated, heat therapy often provides an effective alternative for pain management and tissue healing. Warm compresses can improve circulation, reduce muscle tension, and promote healing in situations where cold therapy would be harmful. However, heat therapy also has its own contraindications and must be applied with appropriate precautions.
The transition from acute injury management to heat therapy requires careful timing and assessment. While cold compress applications are typically recommended immediately following acute injuries, the switch to heat therapy usually occurs after the initial inflammatory phase subsides, typically 48-72 hours post-injury.
Non-Thermal Treatment Options
Compression therapy provides anti-inflammatory benefits without the temperature-related risks associated with cold compress applications. Elastic bandages, compression garments, and pneumatic compression devices can help control swelling and support injured tissues without affecting circulation through temperature changes.
Elevation and rest protocols offer additional non-thermal approaches to injury management. These techniques can be particularly valuable for patients who cannot safely use cold compress therapy due to medical contraindications or environmental factors.
Professional Assessment and Monitoring
Healthcare Provider Evaluation
Complex medical histories require professional assessment before implementing cold compress therapy protocols. Healthcare providers can evaluate multiple risk factors simultaneously and develop individualized treatment plans that account for specific contraindications. This professional oversight becomes particularly important for patients with multiple comorbidities or those taking multiple medications.
Regular monitoring during cold compress therapy helps identify adverse reactions before they become serious complications. Healthcare professionals can establish monitoring protocols and educate patients about warning signs that indicate the need to discontinue cold therapy immediately.
Patient Education and Safety Protocols
Comprehensive patient education about cold compress contraindications empowers individuals to make informed decisions about their treatment options. Patients must understand not only when to avoid cold therapy but also how to recognize signs of complications if cold compress therapy is used inappropriately.
Safety protocols should include clear guidelines about duration limits, temperature controls, and barrier protection to prevent direct skin contact with extremely cold surfaces. These protocols become particularly important for patients with borderline contraindications who may still benefit from modified cold therapy approaches.
FAQ
What medical conditions absolutely prevent cold compress use?
Absolute contraindications for cold compress therapy include severe peripheral vascular disease, active frostbite or cold injury, areas of compromised sensation due to nerve damage, and regions with impaired circulation from any cause. Patients with Raynaud's phenomenon, severe diabetes with neuropathy, and those with open wounds or active infections should also avoid cold compress applications. These conditions significantly increase the risk of tissue damage, delayed healing, or serious complications from cold therapy.
How do age factors affect cold compress safety?
Very young children and elderly patients face increased risks from cold compress therapy due to physiological differences in thermoregulation and skin characteristics. Infants and toddlers have immature temperature control systems and cannot effectively communicate discomfort, while elderly patients often have thinner skin, reduced circulation, and may take medications that affect their response to cold. Both populations require modified treatment protocols or alternative therapies to ensure safety.
Can medications make cold compress therapy dangerous?
Several medication classes can create dangerous interactions with cold compress therapy, including anticoagulants, beta-blockers, calcium channel blockers, and medications affecting circulation. Blood thinners increase bleeding risks, while circulation-affecting medications can either enhance or reduce the vascular response to cold, potentially leading to tissue damage or treatment ineffectiveness. Patients should always consult healthcare providers about potential medication interactions before using cold compress therapy.
What are the warning signs that cold compress therapy should be stopped immediately?
Immediate discontinuation of cold compress therapy is necessary if patients experience severe or increasing pain, skin color changes including white, blue, or mottled appearance, numbness that persists after removal, burning sensations, or any signs of tissue damage. Additionally, if the area becomes excessively stiff, develops blisters, or shows signs of infection, cold therapy should be stopped and medical attention sought promptly.
Table of Contents
- Medical Conditions That Contraindicate Cold Compress Use
- Age-Related Considerations for Cold Compress Avoidance
- Specific Injury Types Requiring Alternative Treatment
- Medication Interactions and Contraindications
- Environmental and Situational Contraindications
- Alternative Treatment Approaches
- Professional Assessment and Monitoring
- FAQ